Statement On Cervical Cancer Awareness By Dr Zanetor Agyeman-Rawlings
Thank you, Right Honourable Speaker for the opportunity to make a statement on cervical
cancer awareness. The month of January is Cervical Awareness Month and the International
Agency for Research on Cancer highlighted three issues, namely vaccinations against Human
Papilloma Virus (HPV) which is the cause of most of the cases of cervical cancer (Mostly
successful in the High income countries, but also shown to be successful in Bhutan).
The second is the treatment of cervical precancerous lesions in a resource constrained setting (there is a study in Zambia using a hand held battery operated device to thermally ablate
precancerous cells) and thirdly, improving coverage of cervical screening programmes in ‘at–risk’ populations. This is derived from the 2018 strategic goal of the World Health
Organisation to eliminate cervical cancer through effective screening, vaccination, and
treatment.

Cervical cancer is the 4 th most common cause of death in women globally
Cervical cancer is the 4 th most common cause of death in women globally; to put that in numbers, that is roughly 311,000 deaths every year. In the year 2020, about 604,000 women were diagnosed with cervical cancer globally and 342,000 women died from same. The high incidence and mortality rates occur in low-and middle- income countries, and Ghana falls within this group.
In Ghana, the incidence rate of cervical cancer is 29.3/100,000 (four times the rate in the
USA) and the mortality rate is 23.8/100,000 (ten times the rate in USA)
Due to the high transmissibility of the covid-19, many routine health services were suspended globally, and cervical screening was no exception. Just as a thought, it might be interesting to do a retrospective study on the impact of the suspension of cervical screening programmes on incidence of the disease in countries that have a national screening programme in place. What is the justification for the establishment of a national screening programme besides the fact that this disease kills too many women, young and old in Ghana! The lack of awareness means that women are presenting too late, resulting in a poor prognosis in a disease that could easily be prevented. To orientate ourselves anatomically, the cervix is the scientific name for the neck of the womb and it has a transformation zone which is a meeting point Dr. Zanetor Agyeman-Rawlings, MP Klottey-Korle between the type of cells that line the inside of the womb and the cells that line the inside of the vagina. (also known as the birth canal). This junction where they meet is called the Transformation Zone; this is where these changes in the cells tend to begin as a precursor to the disease. These precancerous changes that occur in the cervix are easily detected through correct cervical screening, to allow for early intervention with good outcomes. Specifically, with early treatment of any precancerous changes and close monitoring.
Mr. Speaker, if there is one thing we have realised from the mandatory vaccinations that the government rolled out, it is the fact that if there is the desire and political will to roll out a nationwide public health programme, it can be done. Too many statements have been made on the floor of this house with respect to cervical cancer, without it translating into guidance to the executive to come up with a policy that would ensure a nationwide cervical cancer screening programme. Women’s health, and specifically cervical cancer has been relegated to the back bench for too long and we must make a conscious effort to rectify this situation.
Rt Hon Speaker, I will use the Republic of Ireland as case study to illustrate how a country went from a high number of deaths from cervical cancer to a significant decrease in morbidity and mortality related to cervical cancer.
The national cervical screening programme, CervicalCheck
The national cervical screening programme, CervicalCheck, commenced in Ireland in 2008. Free cervical smear tests are offered to over 1.2 million women aged 25-60 every 3 (aged 25-
44) and every 5 year(aged 45-60) years. The reason for the choice of that demographic is cervical cancer takes years to grow, so it’s rare (but not impossible) to develop cervical cancer in your 20s. Most cases are diagnosed between ages 35 and 44. Around 20 percent of cervical cancer cases are diagnosed in women 65 or older. To lower your risk of cervical cancer, you can get the HPV vaccine which targets the specific types HPV 16 and 18, which have been shown to be the most carcinogenic. It is worthy of note, that as more women in the population got vaccinated against HPV 16 and 18, some other genotypes were increasingly found associated with cervical cancer.
Screening was associated with a 60% reduction of cancers in women aged 40, increasing to 80% at age 64. Screening was particularly effective in preventing advanced stage cancers. Conclusions: Cervical screening in women aged 20-24 was shown to have little or no impact on rates of invasive cervical cancer up to age 30. Based on this, in Ireland, anyone with a
cervix who is aged between 25 and 65 is advised to get an HPV cervical screening test when it is due. If aged 25 to 29 years, screening is every 3 years. If aged 30 to 65 years, screening is every 5 years.
Of course, we cannot apply these protocols in Ghana without doing a proper study of cervical cancer cases disaggregated by age to effectively design a policy tailored to our epidemiology.
In 2018, several women in Ireland sued the Health Service Executive, (the equivalent of our Ghana Health Service) after they were given the wrong smear test results for cervical cancer. It is critical to note that a system of this kind is not immune to cyberattacks or mix-ups, and of course the consequences of misdiagnosing a woman are potentially devastating. As these systems are put in place, checks and balances must be instituted, and Standard Operating Procedures strictly adhered to, to reduce these kinds of errors.
National register based on the social security number of each citizen
There is a national register based on the social security number of each citizen, so when the woman turns 25 years of age, she automatically receives an invitation to contact a registered GP or nurse for an appointment to have a free cervical smear, which includes an HPV test. Mr. Speaker, with the digitization and digitalization, underway in our jurisdiction when the NIA finally streamlines and interfaces its database with other agencies, it should be possible to capture every woman on a national register in Ghana that can be used to track and trace all women within the high risk group as part of a policy initiative to reduce the incidence and mortality rates of cervical cancer in Ghana. With the correct algorithm in place, appointment letters can be sent to the correct age groups at the appropriate frequency, as alluded to previously. And with the high mobile phone penetration in Ghana, these invitations can be sent as blast messages to the phones of the women with letters as a back-up and of course, in areas with lower SE situations and poor access, the Community Health Centres (CHPS Compounds) can be sent the list of persons eligible for screening so their community healthcare providers can also follow up in the same way as the childhood vaccinations are done. Additionally, all healthcare personnel who are certified smear takers must be registered with the cervical check to ensure that all data is synced, and no woman gets lost between the cracks. This of course means that very robust cybersecurity systems must be put in place to protect the data of the women on the database.
In addition to the conventional smear tests, there is new technology for cervical screening to prevent cancer:
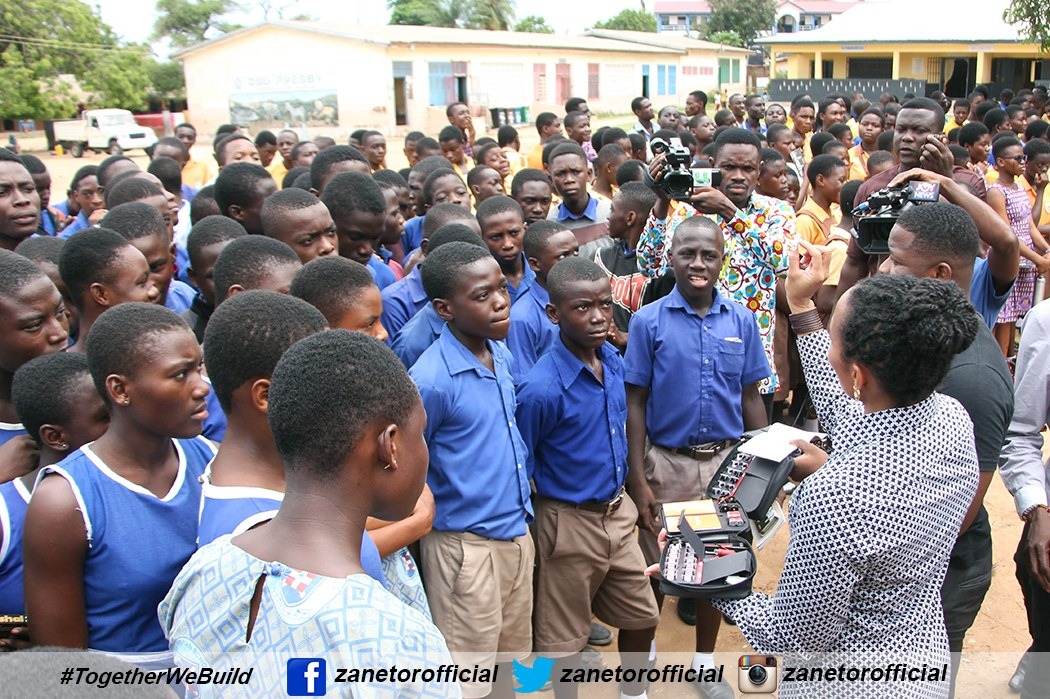
The Israeli company Mobile ODT (Optical Detection Technologies) has designed a tool that removes the need for smear kits and the reagents. This employs the use of software and a smartphone in a mobile colposcope which has been used with great success worldwide. This device has over the years since it was first used accumulated a lot of data which has helped its developers create an AI version which can diagnose conditions well. This means trained healthcare personnel can have immediate results at the primary care level and patients referred appropriately and in a timely fashion.
The bottom line is that there is no need to reinvent the proverbial wheel, however we can certainly adapt it to our unique terrain to ensure the success of the programme. The cost economically and in human lives of setting up a national screening programme for cervical cancer far outweighs the current burden on the health system and the lives lost to cervical cancer in Ghana. The Ghana Health Service has all the data to prove that there is a huge benefit to a nationwide programme. It is my recommendation that the Rt Honourable Speaker refer this to the Committee on Health, for the relevant agencies to brief the members fully on how Ghana can satisfy the WHO goal to eliminate cervical cancer as a public health problem by the year 2030.
Thank you, Mr. Speaker for the opportunity.
References:
https://pubmed.ncbi.nlm.nih.gov
https://iarc.who.int/featured-news/iarc-marks-cervical-cancer-awareness-month-2022/ https://www2.hse.ie/screening-and-vaccinations/cervical-screening/about- cervicalcheck/about.html
| M | T | W | T | F | S | S |
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| 8 | 9 | 10 | 11 | 12 | 13 | 14 |
| 15 | 16 | 17 | 18 | 19 | 20 | 21 |
| 22 | 23 | 24 | 25 | 26 | 27 | 28 |
| 29 | 30 | 31 | ||||






Leave a Reply